Section From Invoice Data Entry Screen
Click here -> to return to the Table of Contents
Invoice Screen
Medicare/Medicaid Windows
SPECIAL STATE-DEPENDENT FIELDS IN THE INVOICE DATA ENTRY SCREEN
Medicare Secondary Modifiers - For Hospital to Hospital
Transports an additional field is required
![]()
Section From Invoice Data Entry Screen
Pressing the F1 Function when the cursor is at the secondary modifier field will display
the following help screen
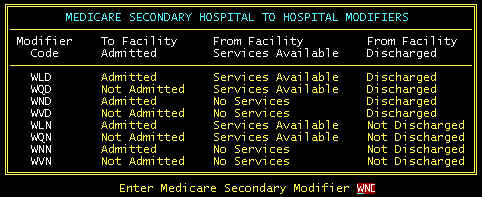
Medicare Secondary Modifier Help Screen
About the only code used is WND-discharged first hospital, admitted second hospital-first
hospital lacks services/facilities.
ENTERING THE PRIMARY AND SECONDARY PAYERS IN THE
INVOICE DATA ENTRY SCREEN
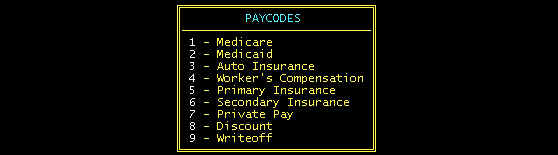
The system uses numbers 1-9 to designate the different type payers, these
numbers we call paycodes. With time, knowing these paycodes will become second
nature. However, at first, you may either need to write these down for reference, or
use the help screen. When your cursor is at one of these paycode fields, pressing
function key F1 will display the following:
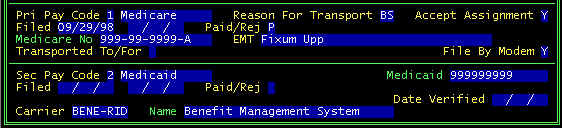
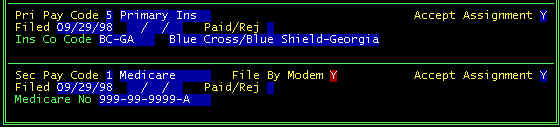
Medicare is the Primary Payer--Window in Invoice Screen
In the primary paycode window, when 1 is entered in the Pri Pay Code
field, the top half of this window is displayed.
Paycode Windows in Invoice Screen
Reason for Transport --
Either enter none, 1, 2 characters per the prompt line at the bottom of the screen, or
press function key F1 for the help screen
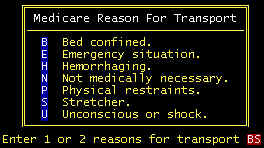
Reason For Transport Help Screen
The following are listed in the order of importance/severity: U, H, E, P/B, S, N.
Note that B is more important than S. always use B when possible, but be prepared to
specifically say why in the secondary diagnosis narrative. Leaving both characters blank
is acceptable, but not advisable.
Accept Assignment -- Participating Providers Must Accept Assignment. This means at least two things: (1) You must accept the Medicare Allowed Amount on the EOB as the total amount you can collect when there is a non-zero allowed amount. Medicare will pay 80% (if there is no deductible), and you are required to attempt to collect 20% from either secondary coverage (coinsurance) or from the patient (copay). (2) Payment comes directly to the ambulance company rather than to the patient.
Filed -- There are two dates, the first is for the first filing, and the second is the refile date.
Paid/Rej(ected) -- Automatically set when posting payments, but can be manually changed here.
Medicare No -- HIC number copied from the patient screen. If you type over the HIC number displayed, this number will permanently replace the one currently in the patient file.
EMT -- the senior EMT for the transport. This is a fairly new requirement by Medicare.
Transported To/For--The prompt line at the bottom of the page will display your (single letter) choices. Pressing the function key F1 will display the help screen below.
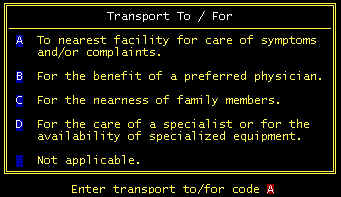
Transported To/For Help Screen
File By Modem - defaulted per the flag in the company screen parameter flags. If Y is in this default, then this will be defaulted here. However, there may be certain claims that need to be filed paper, even though electronic claims being used. If N appears here, this claim will not be extracted for electronic transmission.
Medicare is the Secondary Payer--Window in
Invoice Screen
(see above for screen parameters)
Medicaid
is the Primary Payer-EMERGENCY TRANSPORT
Window in Invoice Screen
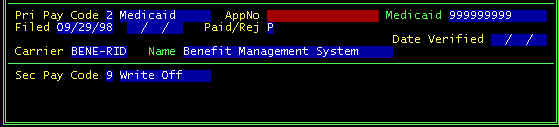
In the primary paycode window, when 2 is entered in the Pri Pay Code field, the top half of this window is displayed.
AppNo (Prior Approval Number)-- Required for non-emergency transports only
Medicaid--Medicaid number extracted from the patient file
Filed--two date fields, the first is first filing date, second field is the refile date
Paid/Rej--Automatically set to either P or R from posting payments, but can be overwritten here
Carrier--Multiple Medicaid Carriers (Intermediaries-HMOs, etc.) are allowed in the program which is the trend in some states. Here, in your insurance company file, you can enter as many (or one) Medicaid Intermediary.
Medicaid
is the Secondary Payer
When Medicaid is the secondary payer, generally they will do what ever the primary does,
using the same charges, HCPCS codes, diagnoses, etc. The invoice window for Medicaid
secondary is shown above-click here