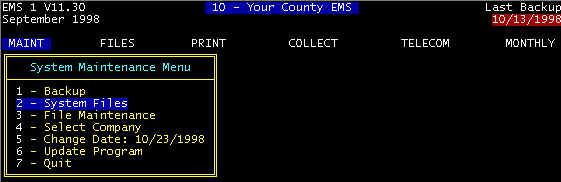
From the Main Menu (screen 1), highlight System Files and
press the <ENTER> key, and the main diagnosis screen is displayed (screen 2).
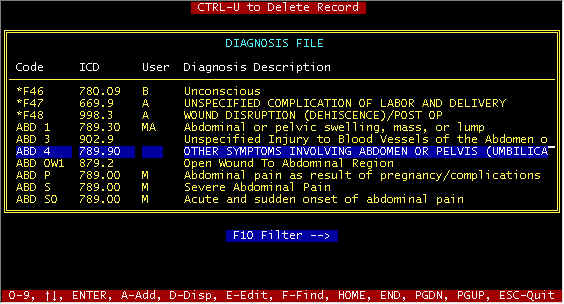
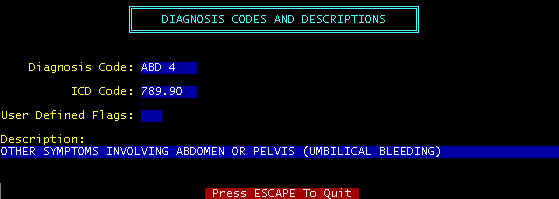
To edit or display a diagnosis in the main diagnosis screen, highlight a diagnosis and
press E(dit) or D(isplay); if the A(dd)
The DIAGNOSIS database file is
a memory bank of diagnoses complete with ICD-9-CM codes. The ICD
codes and descriptions come from official code books to reduce the possibilities of claims
rejections. Most insurance companies request these codes and Most Medicare carriers
require them on electronic claims. The diagnosis database can be added to, and this is
done from time to time to add codes that users feel are needed. The difference between
claims rejections and acceptance many times will depend upon you proving the need for an
ambulance rather than other transportation. Medicare’s rules are simple. Ambulance
necessity falls into two categories: ΠTransport by
means other than ambulance may be detrimental to the patient’s health, and the patient could not SIT. As
already mentioned, the diagnosis database contains ICD codes and descriptions from a
coding manual. However, these were derived for physicians, not ambulances. Normally, you
will use the ICD code and description that most nearly matches the condition
(not necessarily why the ambulance was called). Then, invariably,
(almost invariably) change the extracted wording to match the condition as recorded on the
run sheet--see a sample run sheet in another section. Diagnosis
wording is expanded upon later in this section.
Code Column -- The codes under this column are those that users prefer to
identify with diagnoses, codes that are easy to remember. These are not used for claims
filing, but only for choosing diagnoses (ICD and Descriptions). For example, you may
choose to code all problems involving the arm with ARM1, ARM2, etc. Then, from the invoice
screen when trying to select a diagnosis, entering ARM will not find an exact match, and
the diagnosis file will be displayed alphabetically beginning at the nearest match to your
keyboard entry, and in this case the first line in the main diagnosis screen will be for
ARM1, the second with ARM2, etc. You can highlight your selection, and return is to the
invoice screen with the description and ICD code copied into the invoice screen. If after
choosing a diagnosis, and transferring into the invoice screen, modify the description to
suit the exact situation, while using the same ICD code – do not get too far off base
with disagreement between ICD code and description, as discussed in the Diagnosis
Description paragraph that follows.
ICD Column -- These must exactly match those listed in ICD-9-CM code books.
Note that there are a variable number of characters from one code to another, and ALL
numbers should be used, e.g. 812.01; in the past, Medicare would accept 812 only, but
beginning (approximately) mid to late 1996, Medicare is saying that all numbers must be
used. Print your diagnosis file in order of ICD code, and compare with a
coding manual.
Diagnosis Description Column -- Generally, these descriptions match those in coding manuals,
but not word for word. Diagnosis descriptions are transmitted in what is call the
narrative field. There should be some correlation between the ICD code and the
description, but a single ICD code can fit multiple descriptions, for example w Abdomen Pain, Unspecified; w Acute
Abdomen Pain; w Abdomen Pain due to pregnancy complications,
etc. etc. You would also choose different codes for example: ABDU, ABCAC, ABDP,
respectively for the example descriptions above. Note that all of these code and
description combinations would have the exact same ICD code.
We have covered in general terms the usage of the diagnosis file, but
lets get more specific about coding philosophy and selection of diagnosis codes.
Philosophy of Selecting Diagnoses
If in a medical situation, certain care was
rendered by ambulance personnel in order to prevent further pain and/or injury,
then ambulance necessity was satisfied--most such cases are obvious. Other
than obvious requirements for an ambulance (non-emergency transports e.g.),
ambulance necessity boils down to why an ambulance was required rather than
other transportation (car, taxi, wheelchair/van, etc.). Availability
is not an issue--IF this other transportation were available, COULD the patient
have traveled in that other vehicle--if the answer to that question is YES,
you cannot get paid for the transport. Most emergency transports are
clear cut--the patients condition (unconscious, heart attack, etc.) mandates
special medical care and transport conditions, in which cases what was wrong,
and what you did satisfies ambulance necessity. The problem area is
non-emergency transports. What you have to prove is that THE PATIENT
COULD NOT SIT IN AN ERECT POSITION for the duration of the transport DUE TO
a very specific reason (and you must be SPECIFIC). As mentioned previously,
the Diagnosis database can be added to and modified to some degree to fit
your needs, and you choose the nearest match to your situation and modify
to suit the specifics of this particular transport--diagnosis descriptions
do not have to exactly match those directly from a coding manual, but should
be reasonably in agreement, and not conflicting. You may want to add
diagnosis codes and descriptions without ICD codes, and these can be used
for narratives and phrases that you use frequently and do not want to type
each time--a few examples follow. NON-EMERGENCY
Transports -- These are the most difficult to get paid.
HCFA now requires a Certificate of Medical Necessity Form to be ON
FILE for certain patients--ON FILE means in your filing
cabinet in case you are either audited or requested to submit.. We have
made up a sample Front Side
and Back Side but you may
want to make up your own. There is no official form, each provider makes
their own. As simply as can be stated, a patient under direct care of
a Physician needs the form--this is vague, but that is what the regulation
says. It goes on to say that generally patients transported TO/FROM
residences are usually excluded--again vague. It is a good idea to get this
form filled out for all non-emergency transports--it may be needed to refile
with a HCFA1500 form if you get rejected electronically.
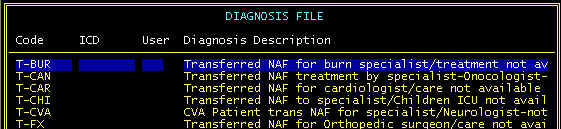
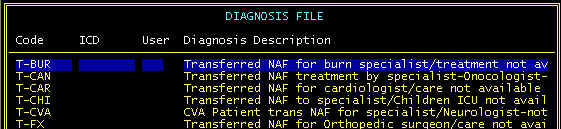
Here we have added our own narratives that can be used in the secondary diagnosis field
for Hospital to Hospital transports and coded these beginning with T- Note
that the description field is wider than can be displayed, but is scrolled when you are in
the EMS program.
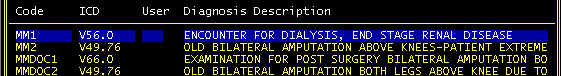
Another special diagnosis you may consider is for frequent flyers, and you
use the same (or a few) diagnoses, depending upon the particular transport that day.
For example, Martha Mayfield may be a dialysis patient. Most transports are
to the dialysis center, but occasionally Martha is transported to a remote specialty
center. You can make up special codes for Martha as shown below.
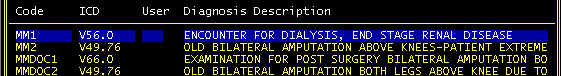
Here MM1 and MM2 are primary and secondary diagnoses for frequent trips to the dialysis
center; MMDOC1 and MMDOC2 are other not-so-frequent to the doctor, but periodic
transports.
One other point – diagnosis descriptions are transmitted in what
is called the narrative field. The way this is done is that the primary diagnosis
description and the secondary diagnosis description are strung together like one long
sentence, with two spaces between the end of the primary and the beginning of the
secondary. Medicare personnel evaluating your claim will see these in this format on their
computer screen, along with other information for the claim. Medicare is looking for one
thing specifically – AMBULANCE NECESSITY
Obviously there needs to be a correct Medicare number, name, etc. as
well as other information, but the difference between approval and rejection will boil
down to AMBULANCE NECESSITY
Assuming you are using an ICD code that reflects the possibility
of AMBULANCE NECESSITY, then your diagnosis descriptions (narrative field) will
make the difference. For example, if you use an ICD code for Fractured Arm, you may get
rejected (I have seen such a rejection), but if you add to the diagnosis description splinting
required to prevent further injury, you are practically assured of approval.
There is a sequence of things to include in your narrative field as
follows:
ΠWhat is Wrong With The Patient
Not what happened –
Blunt Trauma to the Forehead – there is an ICD code with this description. This is
not what is wrong, but what happened. MVA, there are several ICD codes for MVA, but this
is what happened. Instead of Blunt Trauma to the Forehead, your choice of Diagnosis (and
ICD code) is
Severe Laceration to the forehead.
What
happened
If it was Blunt trauma to
the forehead, Add to the diagnosis as follows Severe Laceration to the forehead as a
result of assault with a shovel
Ž What
did the paramedics do that would not have been done via automobile transport
Add further as follows Severe
Laceration to the forehead as a result of assault with a shovel – controlled
bleeding, secured to stretcher due to transient awareness of patient.
Other things to say:
93 yr. old patient – History of CVA – Patient is totally
bedridden, cannot sit, stand, walk – Restraints required due to mental condition
– result of MVA. Medicare may tell you not to include such information, but do
not listen to that and put your best shot in a particular Medicare person reviewing your
claim.
Add to your primary diagnosis (and ICD code) with wording that
reinforces AMBULANCE NECESSITY. Do it for all claims, not just Medicare, because, a
claim that starts out private pay may end up Medicare (if you did not know that it was
Medicare to begin with).
Only Use a Single ICD code--Medicare requires only a single ICD
code. If you give them more, you are possibly giving them conflicting data and possible
grounds for rejection. Instead, load up your primary and secondary diagnosis descriptions
as described above. Ambulance diagnoses differ from physicians in that a physician has the
benefit of X-rays, lab tests, etc. such that a diagnosis code can exactly describe the
situation. Ambulance technicians do not enjoy that luxury, and further do not diagnose,
but instead choose a diagnosis and expand upon it with narrative, as previously described.
Œduring invoice data entry when the
blank primary or secondary diagnosis (code) fields in the invoice screen are reached, and
the ENTER key is pressed with eight or less characters; if less than eight (including
blank), the entry is considered a code, if an exact match is found in the DIAGNOSIS file
(ABD *BV for example), the ICD code (902.9) and diagnosis description (Abdomen .........)
are copied to the invoice screen. Otherwise, the main diagnosis screen is displayed
beginning at the nearest matching code entered, whereupon several search and select
options are available to you.
CTRL-Page Down can be entered at a diagnosis code field,
regardless of field content, and the main diagnosis screen is displayed.
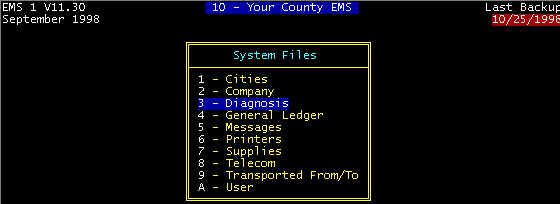
Ž from the menu selections MAINT/System
Files/Diagnosis, as shown, and this is used for adding/editing/displaying diagnoses
Diagnosis File Keyboard Functions and Field
Descriptions
Function Key F10
-- When in the invoice screen, a string of characters entered of length less than 8 into
the diagnosis field will result in searching the diagnosis file for a diagnosis code match
or nearest match. If an exact match is found, the ICD code and description are retrieved
into the invoice screen; otherwise, the nearest matching diagnosis codes and descriptions
are displayed for selection. If the list of displayed nearest matches does not contain a
suitable diagnosis, using F10 will allow you to enter a character string after a which a
window of diagnoses will be displayed with diagnosis descriptions that have that sequence
of characters. For example, note in the main diagnosis screen above that AND is displayed
next to F10-->. This will result in a screen(s) of descriptions with that string, and
will include all with the word HAND, the word GLAND, and there may be
others. This is a powerful feature is searching for diagnoses using key words in the
description fields. If a number is entered instead of a character string, the search will
be for the nearest matching ICD CODE.
CTRL-U to Delete Record -- The highlighted record will be
deleted.
Code -- The diagnosis code is a one to eight character
field that can be either letters or numbers. An attempt has been made to install a
DIAGNOSIS file with (short) code selections that are easy cross-references for (long)
diagnostic descriptions, as described immediately above. Diagnostic codes can be changed
by users to suit individual preferences; if another code system works better, change these
codes. However, use caution in changing ICD codes and diagnostic descriptions that are not
compatible with official ICD code books.
ICD -- As described above, this is the ICD.9.CM code
required by Medicare and most insurance companies. Do not change these codes unless there
is a directive from Medicare. The same ICD code and description can be used with more than
one diagnosis code; for example HED CUT and FAC CUT could both have the same ICD code and
description since the face (FAC) falls into the head (HED) category.
Diagnosis Description -- These descriptions match those
listed in code books. To be consistent, as well as using wording that is less likely to be
misunderstood by paper claims processors, take care in drastically editing this Diagnosis
Description field. EMT's and Paramedics legally cannot diagnose, and thus it may be best
to preface some diagnosis descriptions with "possible"; e.g. possible fracture;
possible stroke. Sometimes the patient complains of, e.g. abdominal pain or chest pain,
and these do not require the "possible" preface word.
Arrow Keys(¯),HOME,
END, PGDN, PGUP -- These key entries reposition the cursor and/or pointer position
in the file, and well as change the display accordingly. As previously described, the
arrow keys can be used to highlight a diagnosis.
HOME - jumps to the beginning of the DIAGNOSIS file and displays
the first 10 diagnoses
END - jumps to the end of the file and displays the last 10
diagnoses
PGDN - jumps 10 down in the file and displays next 10
PGUP - jumps 10 up in the file and displays and displays
previous 10
ENTER KEY -- The <ENTER> key is used: t to select the highlighted diagnosis when the screen was
displayed when branching from the invoice screen. t
to terminate a keyboard string entry as a result of A-Add, E-Edit, F-Find, and
F-->Filter function selections
A-Add, D-Display, E-Edit -- From the main screen, results
in the appropriate detail screen display.
F-Find -- Similar to F10->Find that searches for a
string-match in the description field, F-Find searches the code
field. A prompt will be displayed allowing entry of a string of code characters to be
entered, after which the window will display codes beginning with the nearest (or exact)
match.
ESC-Quit -- Pressing the ESCape key branches back to the
previous screen with data entry, changes, etc. aborted and no action taken such that all
files, data fields, etc. remaining in the same condition as before entering the screen.
CTRL-END to Save -- The CTRL-END key entry will save and
exit a screen data entry at any field position, in some cases. If a screen contains
necessary unfilled fields, the entry is aborted (with a message display) and the next
(from the top) required field is highlighted. Successively pressing the <ENTER> key
past the last data field will also save data on the screen.