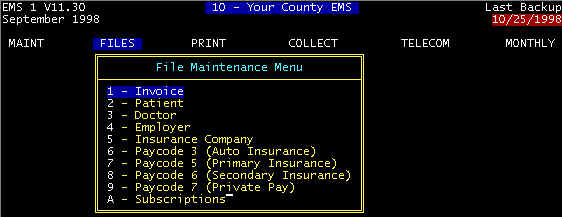
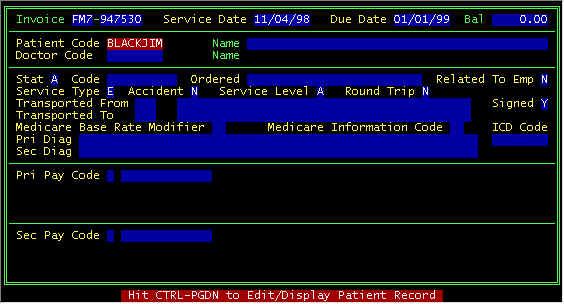
Screen 1
ê
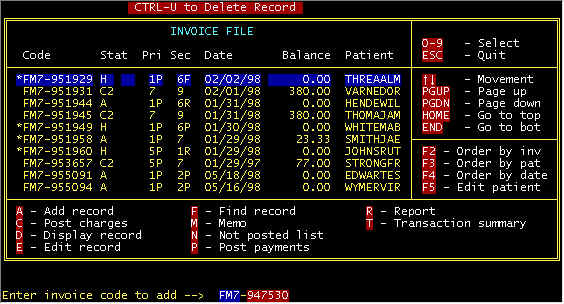
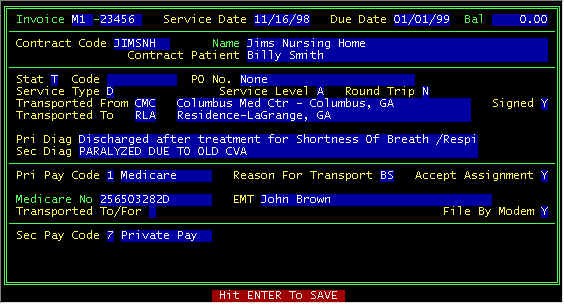
Screen 2 - Main Invoice Screen
Letter A key was pressed (A-Add record), and
at the bottom, a prompt line is displayed with a blank invoice number for key entry -- for
the example above, FM7 and 947530 were entered into the two fields. Then a (mostly)
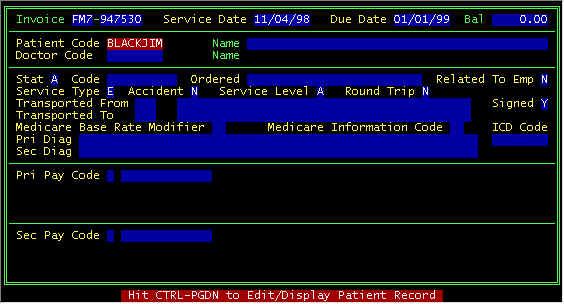
blank detail invoice screen is displayed with the invoice number that was entered and the
service date defaulted to yesterday's date. Either press the <ENTER> key to
accept the service date
or type over the default date. The computer will calculate a due date which will be the first of a
subsequent month, and you can either accept or type over -- NOTE
-- payment status, etc. plus this due date will affect the severity of statement messages,
as described in the section POST PAYMENTS.
Bal(ance Due) will show
total balance for all invoices this patient, once the patient code is entered. Next, make
up a patient code
from the patient's name, for example BLACKJIM for Jim Blackstone -- 5 characters of the
last name plus 3 characters of the first name. This is not etched in stone, but we
have found that this scheme results in insignificant duplication for different people with
similar names.Once the patient has been either entered or retrieved (already on file), the
patient name is
retrieved from the patient data base.
ê
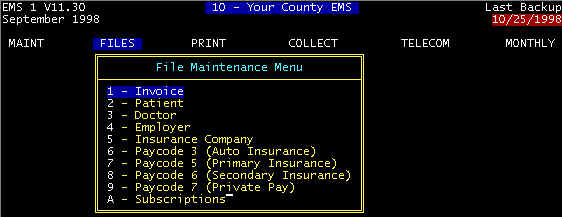
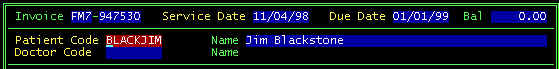
Screen 3 - Detail Invoice Screen
After entering a patient code, one of 2 things will happen:
if the patient is on file and has an existing invoice on file, the one
with latest date of service will have that invoice data imported into screen 3 above, and
you can change the date of service, and other data specific to THIS trip. Charges,
payments, memos, are not imported, and the status is set of A-Active. This is useful
for frequent flyers, plus patients you previously transported to the hospital, and this is
the return trip. If the trip to the hospital was CVA, then modify the diagnosis
description by adding: Discharged after treatment for...............
if the patient is not on file, the program branches to the patient
screen, shows a window of nearest matches to the patient code you have entered, for either
selecting one displayed or selecting A-Add (patient), as described in PATIENT section.
After a patient has been selected/new one entered, the top part of your
screen will look like this
ê
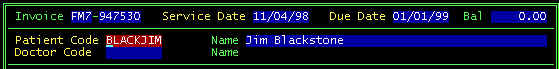
Screen 4 - Detail Invoice Screen After patient
selection
Doctor Code--(See
the DOCTOR Database).
The next field to enter is either the attending physician of the
referring physician. Once the doctor has either been entered,
the doctor name
is retrieved and displayed. Often times, an ambulance service
transporting a patient to a hospital and/or some facility does not
know the physician, and thus, often we will use something like ER
Doctor-County Hospital, and more of your screen is filled in as
follows:
ê
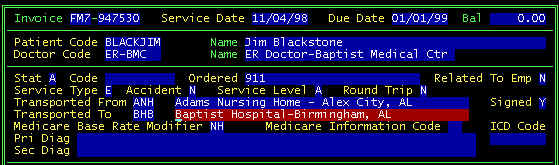
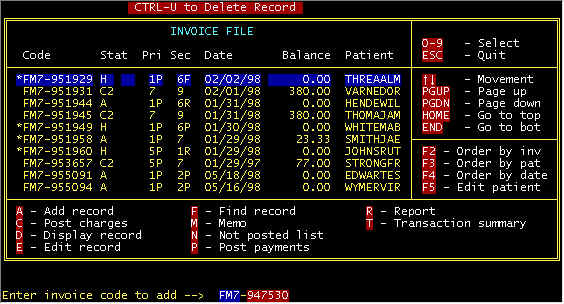
Screen 5 - Detail Invoice Screen Data Entry
Continuing the data entry -- On a new invoice, the default Stat(us) is A-Active, but
later may change. When your cursor is at this field, a prompt line will be displayed
at the bottom of your screen as follows:
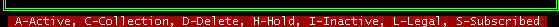
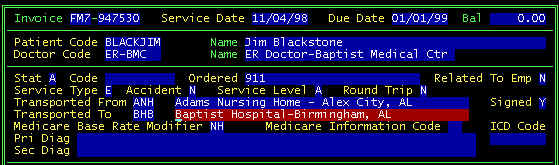
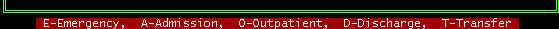
Screen 6 - Detail Invoice Screen Prompt Line-Invoice
Status
The Code
field is free form, and on a new invoice is usually left blank -- this field is discussed
more in the field descriptions section of the INVOICE
screen in another section.
Ordered -- Who called
the ambulance - Family, Bystander, via 911, etc.
Related To Emp(loyment)--
Workman's Comp?
Service Type--screen
below is displayed on your prompt line when the cursor is at this field
Screen 7 - Detail Invoice Screen Prompt Line-Service
Type
E-Emergency--This is the only selection that is classified as an
emergency transport; all others are non-emergence. Thus, not select T-Transfer for
hospital to hospital transports, when the patient is in a health threatening situation
(EKG, IV, etc. enroute)--use Emergency for these type transports.
O-Outpatient--These are for local trips (nursing home to Physician Office-Clinic, and to
hospital) where the patient is not discharged first facility, admitted second
facility. T-Transfer--this is non-emergency facility to facility transport,
discharged first facility, admitted second facility.
Accident
-- Two types (Auto) and (2) non-auto your prompt line is shown below

Screen 8 - Detail Invoice Screen Prompt Line-Accident
(enter Y, N, or A)
Service Level --
A-ALS, B-BLS. Some states may argue the point as to what is ALS and BLS, but the ALS/BLS
is not what you do, it is ambulance and crew. Prior to 1995, some services
were allowed to charge all ALS if trucks and crews qualified PLUS
there was a local ordinance mandating all ALS. On January 1, 1995 HCFA
addressed this problem and instituted four ALS codes-two emergency and two non-emergency,
away from the single ALS code (A0220) which was the highest reimbursed.HCFA initiated two
non emergency ALS codes intended to reduce Medicare reimbursements, but it backfired, and
reimbursements went up. On the Federal Register about October 1997 HCFA listed
proposed legislation (for comment) to fix their previous fix, and defining about 50
ICD codes (diagnoses) for ambulance services with those where ALS is allowed, and those
that can only be BLS--these are listed on our Sample Run Sheet.
There has been some controversy about these codes. For example, HCFA proposes a hand
injury to be ALS, but unconscious can only be BLS - does not take a Ph.D. physician to see
the absurdity in this. To summarize ALS versus BLS, different states could interpret
this however they wish-good luck.
Round Trip--if
Y(es), a field will be displayed for the return vehicle, plus when charges are posted, the
return HCPCS codes will be posted with the base rate modifiers reverse (Residence to
hospital modifiers--going RH, return HR). Round trips are to and return the same day.
You may choose to code round trips as two trips. However, beginning January
1, 1999, Medicare nursing home patients in Part A stay may require coding it as one claim.
Transported Form/To--A
database can be user-defined with local transport locations and
facilities such that a 1-3 character input at an address data input field will pull
in City, State, Zip, Area Code in order to reduce data entry. However, this coed is
not necessary, and the locations can be manually entered. The advantage of using the
database and codes is that base rate modifiers are automatically assigned (see FROMTO). In
the screen above, the code BHB was entered and Baptist Hos........... was retrieved.
If you cannot remember a code, a Ctrl-PageDown (Hold the Ctrl and tap the PageDown key)
will get you to the FROM/TO file for viewing, searching, selection, adding a new one.
Signed -- Did the
patient sign the run sheet: Yes or No. This message will not show here if programmed
in the Company Screen parameters. For a sample of the
statements you may choose to have the patient sign, see the statement (taken from what
some hospitals require) on our Sample Run Sheet.
Medicare Base Rate
Modifiers -- immediately above, it was stated that base rate modifiers
are automatically assigned for transport locations in the FROM/TO
database--here, NH have been assigned and will be attached to the HCPCS (A0330NH) for
claims submission. For a more detailed description of Base Rate Modifiers, go to the
FROMTO section.
Medicare Information
Code--This will be specific to each state and is a secondary HCPCS
modifier. Different states may or may not have secondary modifiers, and will call
them some other than Medicare Information Code. When you put your billing state in company screen 1, your screens are configured to
suit that specific state. Here, you are seeing the configuration for Alabama.
Click HERE to
see special secondary modifiers specific to your state, as well as Medicare and Medicaid
differences. When you come to this data entry field in the invoice screen, pressing
Function key F1 will display your choices.
Primary
and Secondary Diagnoses
Philosophy for coding diagnoses, using the search engines, etc. are discussed in detail in
the DIAGNOSIS section. To summarize here, the diagnosis data
base has one record per diagnosis, with multiple fields per record, as shown below.
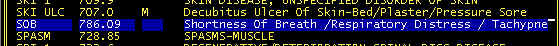
Screen 9 - Diagnosis screen-Sample display
Here, the user has defined a short code they can remember SOB (Shortness
of Breath). When the cursor is at the beginning of either diagnosis field in the
invoice data entry screen, entering less than eight characters is a signal to the computer
that this is not a diagnosis, but a user-defined code, and the description and ICD code
are extracted from the diagnosis database. For more details, examples, and special
cases, go to the DIAGNOSIS section.
Primary
and Secondary Pay Codes
The system uses 9 payor categories as follows:
Click on one of the
categories above for a detailed description
There is a priority chain of payers. Payment filing and responsibilities
trickle down from the Primary payer, once the primary payment has resolved. Private Pay is
the last (and defaulted) when there is some type Medicare. Insurance, etc. coverage.
Payment from secondaries are not considered due until the primary payers have either paid
or rejected. Three examples of Medicare patients follow:
Medicare Patient With No Secondary Coverage -- The
patient will not receive statements saying you owe until
Medicare has either paid or rejected. In other words, after the primary has been resolved,
payment trickles down to the next payer, and in this case it would be private pay (the
patient).
Medicare Patient With secondary MEDIGAP insurance --
When the Medicare claim is filed, the secondary (crossover) MEDIGAP insurance is also
filed to Medicare and along with the Medicare claim. Medicare files the secondary
for you, and no more filing is required. The patient will not receive statements
saying you owe unless there is a balance after Medicare and
MEDIGAP pay/reject.
Medicare Patient With non-MEDIGAP secondary insurance. When the
Medicare claim is filed, the secondary will not be filed. After receiving
payment/rejection, the secondary insurance is filed (HCFA1500 form) with a copy of the
Medicare EOB (Explanation of Benefits). Similar to above, the patient payment
responsibility will be after resolution of the secondary payer if there is still a balance
due.
|